Historical Medicaid spending in Montana
![]() This article does not contain the most recently published data on this subject. If you would like to help our coverage grow, consider donating to Ballotpedia.
This article does not contain the most recently published data on this subject. If you would like to help our coverage grow, consider donating to Ballotpedia.
| Healthcare policy in the U.S. |
|---|
| Obamacare overview |
| Obamacare lawsuits |
| Medicare and Medicaid |
| Healthcare statistics |
Montana's Medicaid program provides medical insurance to groups of low-income people and individuals with disabilities. Medicaid is a nationwide program jointly funded by the federal government and the states. Medicaid eligibility, benefits, and administration are managed by the states within federal guidelines. A program related to Medicaid is the Children's Health Insurance Program (CHIP), which covers low-income children above the poverty line and is sometimes operated in conjunction with a state's Medicaid program. Medicaid is a separate program from Medicare, which provides health coverage for the elderly.
Background
Established in 1965, Medicaid is the primary source of coverage for low-income and disabled individuals and the largest source of financing for the healthcare services they need. In 2014, about 80 million individuals were enrolled in Medicaid, or 25.9 percent of the total United States population. According to the Kaiser Family Foundation, Medicaid accounted for one-sixth of healthcare spending in the United States during that year.[1][2][3]
The federal Centers for Medicare and Medicaid Services (CMS) monitors state Medicaid programs and establishes requirements for service delivery, quality, funding, and eligibility standards. Medicaid does not provide healthcare directly. Instead, it pays hospitals, physicians, nursing homes, health plans, and other healthcare providers for covered services that they deliver to eligible patients.[3][4]
The Patient Protection and Affordable Care Act of 2010, also known as Obamacare, provided for the expansion of Medicaid to cover all individuals earning incomes up to 138 percent of the federal poverty level, which amounted to $16,643 for individuals and $33,948 for a family of four in 2017. A 2012 United States Supreme Court decision made the Medicaid expansion voluntary on the part of the states.[5][6]
Benefits
In large part, the states "determine the type, amount, duration, and scope" of benefits offered to individuals enrolled in Medicaid, according to the Centers for Medicare and Medicaid Services. However, benefits are subject to federal minimum standards. The federal government has outlined 16 benefits that are required of all Medicaid programs:[7][8][9]
- Hospital services for inpatients
- Hospital services for outpatients
- Health screenings for individuals and children under age 21
- Nursing facility care
- Home healthcare
- Physician checkups and other services
- Rural health clinic visits
- Visits to federally qualified health centers
- Laboratory tests and X-rays
- Family planning
- Nurse midwife care
- Maternity and newborn care
- Visits to pediatric and family nurse practitioners
- Visits to licensed freestanding birth centers
- Emergency and non-emergency medical transportation
- Tobacco cessation programs for pregnant women
Optional benefits offered in Montana
In addition to the above required benefits, as of 2012, the optional benefits included in the bulleted list below were offered in Montana, according to the Henry J. Kaiser Family Foundation. Note that other, less common specialized practitioner services may also have been offered, such as nutritionists and acupuncturists.[9][10]
| Number of benefits offered | ||||||
|---|---|---|---|---|---|---|
| Montana | 42 | |||||
| North Dakota | 45 | |||||
| South Dakota | 43 | |||||
| Wyoming | 41 | |||||
- Freestanding ambulatory surgery centers
- Public and mental health clinics
- Certified registered nurse anesthetists
- Dental care
- Dental surgery
- Optometrists
- Podiatrists
- Psychologists
- Occupational therapy
- Physical therapy
- Speech/hearing/language therapy
- Dentures
- Eyeglasses
- Hearing aids
- Home medical equipment
- Prosthetics
- Adult health screenings
- Case management
- Home and community-based services
- Hospice care
- Personal care
- Inpatient psychiatric care for individuals under age 21
- Inpatient care for mental diseases for individuals age 65+
- Intermediate care for intellectual disabilities
State and federal spending
During fiscal year 2012, combined federal and state spending for Medicaid was higher in Montana than in its neighboring states, totaling about $973 million. Per enrollee spending amounted to $8,840, below only that of North Dakota. The federal government accounted for about 68 percent of spending, while the state government was responsible for 32 percent. Between 2000 and 2012, Medicaid spending in Montana grew by 67 percent, or about 4.4 percent per year.[11][12][13][14][15]
| Medicaid spending, fiscal year 2012 | |||||||
|---|---|---|---|---|---|---|---|
| State | Total spending*† | Per enrollee*† | Total growth‡ | Compound annual growth rate‡ | Federal share* | State share* | Percent of state budget |
| Montana | $972,565,512 | $8,840 | 67% | 4.4% | 68% | 32% | 16.8% |
| North Dakota | $744,160,777 | $11,469 | 37% | 2.6% | 56% | 44% | 12.1% |
| South Dakota | $749,271,225 | $6,969 | 50% | 3.4% | 63% | 37% | 20.9% |
| Wyoming | $528,478,993 | $7,713 | 86% | 5.3% | 51% | 49% | 9.5% |
| United States | $415,154,234,831 | $5,790 | 63% | 4.1% | 57% | 43% | N/A |
| * "Expenditures do not include administrative costs, accounting adjustments, or the U.S. Territories." † Includes both state and federal expenditures. ‡ 2000–2012. Includes payments for services, administrative expenses, and DSH payments. | |||||||
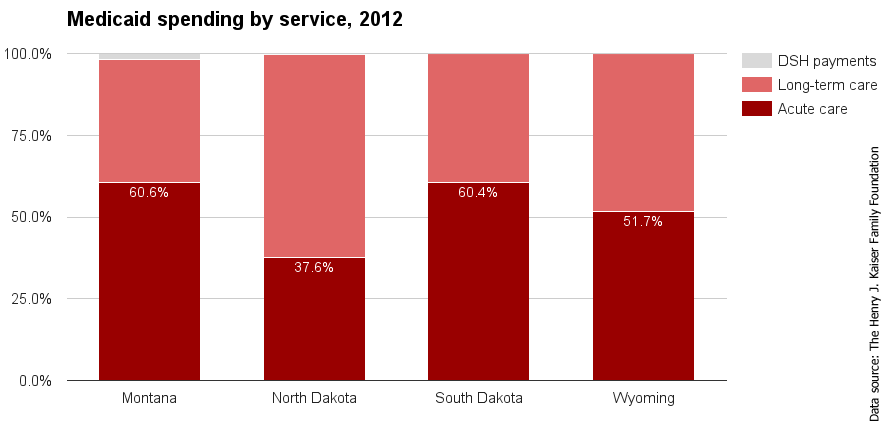
Acute care services are those that are typically provided within a short time frame, such as inpatient hospital stays, lab tests and prescription drugs. Long-term care services, on the other hand, are those provided over a long period of time, such as home care and mental health treatment. Disproportionate Share Hospital (DSH) payments are funds given to hospitals that tend to serve more low-income and uninsured patients than other hospitals. The bulk of Montana’s total Medicaid spending went to acute care services, a greater portion than in neighboring states. A greater portion was also spent on DSH payments in Montana at 1.8 percent. The remaining 37.7 percent went to long-term care services.[16]
| Back to top↑ |
Enrollment
According to a July 2014 report from the Pew Charitable Trusts, in 2010 there were 128,792 Montana residents enrolled in Medicaid. By 2013, Medicaid covered 12 percent of Montana residents; between 2000 and 2012, this figure had increased by 2.3 percentage points.[17][18]
In 2010 the majority of spending, 65 percent, was on the elderly and disabled, who made up 25 percent of Medicaid enrollees. This was typical of most states, since this group of enrollees is "more likely to have complex health care needs that require costly acute and long-term care services," according to the Pew Charitable Trusts. The portion of Medicaid enrollees who are elderly and disabled is a factor taken under significant consideration when state lawmakers make appropriations for the program each year.[19]
| Distribution of Medicaid enrollment and payments, 2010 | ||||||
|---|---|---|---|---|---|---|
| State | Enrollment rates | Payment for services | ||||
| Total | Elderly and disabled individuals | Parents and children | Total (in billions) | Elderly and disabled individuals | Parents and children | |
| Montana | 128,792 | 25% | 75% | $0.9 | 65% | 35% |
| North Dakota | 82,762 | 26% | 74% | $0.7 | 74% | 26% |
| South Dakota | 133,739 | 23% | 77% | $0.8 | 61% | 39% |
| Wyoming | 87,433 | 20% | 80% | $0.5 | 66% | 34% |
| United States | 66,390,642 | 24% | 76% | $369.3 | 64% | 36% |
| Source: The Pew Charitable Trusts, "State Health Care Spending on Medicaid" | ||||||
Dual eligibility
- See also: Medicaid and Medicare dual eligibility
Enrollment
Some individuals, such as low-income seniors, are eligible for both Medicare and Medicaid; these individuals are known as dual-eligible beneficiaries. For those enrolled in Medicare who are eligible, enrolling in Medicaid may provide some benefits not covered by Medicare, such as stays longer than 100 days at nursing facilities, prescription drugs, eyeglasses, and hearing aids. Medicaid may also be used to help pay for Medicare premiums. According to the Henry J. Kaiser Family Foundation, in 2011 there were 19,700 dual eligibles in Montana, or 15 percent of Medicaid enrollees. While average Medicaid spending per enrollee was $7,140, spending per dual eligible was $24,206.[20][21][22][23][24]
| Dual eligible enrollment, fiscal year 2011 | |||||||
|---|---|---|---|---|---|---|---|
| State | Total Medicaid enrollment | Medicaid spending per enrollee | Number of dual eligibles | Dual eligibles as a percent of Medicaid enrollees | Medicaid spending per dual eligible | ||
| Montana | 105,900 | $7,140 | 19,700 | 15% | $24,206 | ||
| North Dakota | 65,100 | $8,338 | 16,300 | 19% | $29,027 | ||
| South Dakota | 102,300 | $5,485 | 22,100 | 16% | $13,835 | ||
| Wyoming | 67,200 | $6,110 | 11,600 | 13% | $26,403 | ||
| United States | 53,535,000 | $5,790 | 9,972,300 | 15% | $16,904 | ||
| Source: The Henry J. Kaiser Family Foundation, "State Health Facts" | |||||||
Spending
Total Medicaid spending for dual eligibles in Montana amounted to almost $400 million in 2011. Most payments were made toward long-term care.[25]
| Medicaid spending for dual eligibles by service, fiscal year 2011 (in millions) | ||||||
|---|---|---|---|---|---|---|
| State | Medicare premiums | Acute care | Prescribed drugs | Long-term care | Total | |
| Montana | $27 | $71 | $2 | $299 | $399 | |
| North Dakota | $11 | $42 | $2 | $348 | $402 | |
| South Dakota | $27 | $45 | $1 | $191 | $264 | |
| Wyoming | $6 | $75 | $1 | $176 | $258 | |
| United States | $13,489 | $40,190 | $1,462 | $91,765 | $146,906 | |
| Source: The Henry J. Kaiser Family Foundation, "State Health Facts" | ||||||
| Back to top↑ |
Children's Health Insurance Program (CHIP)
In 2015, Montana served CHIP enrollees through a combination of Medicaid and a separate program. Its upper eligibility limit was 266 percent of the FPL, meaning a family of four had to make less than $63,441 per year to qualify. The state imposed cost sharing beginning at 142 percent of the FPL]. Below is a table with some general information about CHIP in Montana, including spending figures, the state's federal match percentage, and enrollment in the program. These data points are compared with those of its neighboring states.[26][27][28][29][30][31]
| General CHIP information for Alabama | |||||||
|---|---|---|---|---|---|---|---|
| State | Total CHIP expenditures, 2015 (millions) | Enhanced FMAP, 2017* | CHIP enrollment, 2014 | Program type | |||
| Federal | State | Total | |||||
| Montana | $69.80 | $21.90 | $91.70 | 98.89% | 49,671 | Combination | |
| North Dakota | $14.50 | $7.80 | $22.30 | 88.00% | 5,032 | Combination | |
| South Dakota | $16.30 | $8.40 | $24.70 | 91.46% | 15,870 | Combination | |
| Wyoming | $7.80 | $4.20 | $12.00 | 88.00% | 9,095 | Separate CHIP | |
| United States | $9,528.00 | $3,933.40 | $13,461.40 | 88.00% | 8,129,426 | N/A | |
| * FMAP stands for Federal Medical Assistance Percentage and reflects the percentage of state dollars spent on CHIP that are eligible for matching funds from the federal government. Sources: The Henry J. Kaiser Family Foundation, "State Health Facts" MACPAC, "CHIP Spending by State" | |||||||
See also
Medicaid in the 50 states
Click on a state below to read more about the Medicaid program in that state.
Footnotes
- ↑ The Kaiser Commission on Medicaid and the Uninsured, "Medicaid Enrollment in 50 States," February 2010 (Note 1)
- ↑ Center on Budget and Policy Priorities, "Policy Basics: Introduction to Medicaid," June 19, 2015
- ↑ 3.0 3.1 The Henry J. Kaiser Family Foundation, "Medicaid Financing: How Does it Work and What are the Implications?" May 20, 2015
- ↑ Centers for Medicare and Medicaid Services
- ↑ Kaiser Health News, "Consumer’s Guide to Health Reform," April 13, 2010
- ↑ Office of The Assistant Secretary for Planning and Evaluation, "Poverty Guidelines," accessed June 9, 2017
- ↑ Medicaid.gov, "Benefits," accessed June 8, 2017
- ↑ The Commonwealth Fund, "Medicaid Benefit Designs for Newly Eligible Adults: State Approaches," May 11, 2015
- ↑ 9.0 9.1 The Henry J. Kaiser Family Foundation, "KCMU Medicaid Benefits Database: General Benefits and Cost-Sharing Notes," January 2014
- ↑ The Henry J. Kaiser Family Foundation, "Medicaid Benefits Data Collection," accessed September 24, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Total Medicaid Spending," accessed July 17, 2015
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedperenrollee - ↑ The Pew Charitable Trusts, "State Health Care Spending on Medicaid" Table B.1, accessed July 17, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Federal and State Share of Medicaid Spending," accessed July 17, 2015
- ↑ National Association of State Budget Officers, "State Expenditure Report: Examining Fiscal 2011-2013 State Spending: Table 5," accessed July 17, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Distribution of Medicaid Spending by Service," accessed July 17, 2015
- ↑ Data on Medicaid enrollment figures may differ depending on the source of data and the computational methods used, such as "point-in-time" figures versus "ever-enrolled" figures.
- ↑ Centers for Medicare and Medicaid Services, "Total Medicaid Enrollees - VIII Group Break Out Report," accessed September 14, 2015
- ↑ The Pew Charitable Trusts, "State Health Care Spending on Medicaid," July 2014
- ↑ The Henry J. Kaiser Family Foundation, "Monthly Medicaid Enrollment (in thousands)," accessed September 4, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Medicaid Spending per Enrollee (Full or Partial Benefit)," accessed September 4, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Number of Dual Eligible Beneficiaries," accessed September 4, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Dual Eligibles as a Percent of Total Medicaid Beneficiaries," accessed September 4, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Medicaid Spending per Dual Eligible per Year," accessed September 4, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Distribution of Medicaid Spending for Dual Eligibles by Service (in Millions)," accessed July 17, 2015
- ↑ The Henry J. Kaiser Family Foundation, "Medicaid and CHIP Income Eligibility Limits for Children as a Percent of the Federal Poverty Level," accessed May 25, 2016
- ↑ The Henry J. Kaiser Family Foundations, "Premiums, Enrollment Fees, and Cost-Sharing Requirements for Children," accessed May 26, 2016
- ↑ Medicaid and CHIP Payment and Access Commission, "CHIP Spending by State," accessed May 26, 2016
- ↑ The Henry J. Kaiser Family Foundation, "Enhanced Federal Medical Assistance Percentage (FMAP) for CHIP," accessed May 26, 2016
- ↑ The Henry J. Kaiser Family Foundation, "CHIP Program Name and Type," accessed May 26, 2016
- ↑ The Henry J. Kaiser Family Foundation, "Total Number of Children Ever Enrolled in CHIP Annually," accessed May 26, 2016