Pay-for-performance
This article does not receive scheduled updates. If you would like to help our coverage grow, consider donating to Ballotpedia. Contact our team to suggest an update.
| Healthcare policy in the U.S. |
|---|
| Obamacare overview |
| Obamacare lawsuits |
| Medicare and Medicaid |
| Healthcare statistics |
Pay-for-performance in healthcare is a third-party reimbursement model that uses incentives to encourage providers to improve the quality and cost of care. In pay-for-performance arrangements, doctors and hospitals are scored on a variety of measures and typically awarded a financial bonus for meeting quality and efficiency targets; some arrangements also impose penalties for failing to meet the specified targets.
The Affordable Care Act of 2010 significantly expanded the use of pay-for-performance reimbursement models by Medicare. One of the more expansive programs is the accountable care organization, which is a network of hospitals and physicians of different specialties that coordinate patient care as a unit and are reimbursed on a pay-for-performance basis. About 24 million individuals are cared for by accountable care organizations nationwide.
Overview
Pay-for-performance in healthcare is a third-party reimbursement model that uses incentives to encourage providers to improve the quality and cost of care. Pay-for-performance models are adopted by private and public payers alike as an alternative to fee-for-service reimbursement, in which doctors are paid for each treatment, test, and office visit. A few different program features fall under the umbrella term of pay-for-performance.[1][2]
In most pay-for-performance arrangements, doctors receive a reward in addition to their regular pay for meeting predetermined quality and efficiency measures. Sometimes physicians are also rewarded for improvement over time, even if targets are not met. The incentive or reward in pay-for-performance arrangements is typically a financial bonus, but can also take the form of greater overall payments or having a greater number of a health plan's enrollees directed to the physician's office. Pay-for-performance arrangements also sometimes penalize physicians for failing to meet quality and efficiency targets. Pay-for-performance incentives are compatible with either fee-for-service reimbursement or other reimbursement models, such as bundled payments, in which "providers receive a budget to take care of their patients rather than payments for separate services."[2][3]
Measures used to determine physician performance in pay-for-performance arrangements vary by program and may fall into any of the following categories:[2][4]
- Process (e.g. "whether or not aspirin was given to heart attack patients")
- Service utilization/cost management
- Patient experience/satisfaction
- Patient safety
- Administrative structures (e.g. health information technology adopted by the practice, such as electronic health records)
- Health outcomes
Due to the compounding factors that influence health outcomes, basing pay-for-performance reimbursement on such outcomes is more controversial than the other metrics.[2]
According to Health Affairs, over 40 pay-for-performance programs were in use in the private sector in 2012. In the public sector, many states have implemented pay-for-performance reimbursement models in their Medicaid programs, although the exact number is unclear. Additionally, the Affordable Care Act of 2010 significantly expanded the use of pay-for-performance reimbursement models in the public sector.[2]
Affordable Care Act
- See Ballotpedia's Affordable Care Act overview to learn more about the law.
The Affordable Care Act of 2010 established a number of new programs for Medicare that utilize pay-for-performance reimbursement models. Although "[s]ome are not, strictly speaking, pay-for-performance programs," they all attempt to link reimbursement to quality.[2][5]
- Hospital Value-Based Purchasing Program
- In the Hospital Value-Based Purchasing program, hospitals can receive a bump in their reimbursement from Medicare based on their performance on a set of quality measures. The bonus hospitals receive may be for "[h]ow well they perform on each measure compared to all hospitals" or for showing improvement over time compared to their own previous performance. The amount of the bonus may be higher the better the performance.[2][5]

- Medicare Advantage
- Under the Affordable Care Act, Medicare Advantage plans, which are private health plans financed by Medicare, can receive bonuses based on quality ratings. The Centers for Medicare and Medicaid Services (CMS) established a trial run of the bonus program. Medicare Advantage plans will receive a bonus in their payments from Medicare if they receive at least three out of five stars on a quality-rating scale. Bonuses are greater for plans that receive four or more stars.[2]
- Hospital Readmissions Reduction Program
- While not strictly a pay-for-performance program, the Hospital Readmissions Reduction Program allows Medicare to reduce payments to hospitals that have a high rate of preventable readmissions. The payment reduction amounted to 1 percent in 2013, 2 percent in 2014, and percent in 2015.[5][6]
- Hospital-Acquired Condition Reduction Program
- In the Hospital-Acquired Condition Reduction Program, Medicare may reduce payments to certain hospitals "that rank in the worst performing quartile" for their rate of hospital-acquired conditions. CMS determines which hospitals will see reduced payments by calculating a score based on the following:[5][7]
- a composite of quality measures from the Agency for Healthcare Research and Quality,
- the rate of bloodstream infections,
- the rate of urinary tract infections caused by catheters, and
- the rate of surgical infections.
Accountable care organizations
Accountable care organizations (ACOs) were established on a trial basis by the Affordable Care Act as a new healthcare delivery model for Medicare providers. An ACO is a network of hospitals and physicians of different specialties that "work together to save money by giving more efficient medical care to their patients." ACOs are reimbursed on a pay-for-performance basis. If an ACO spends less money treating Medicare patients than it did previously, then the ACO receives a bonus on its reimbursement. If not, the group will have to take a loss on the cost of care provided to those patients. Bonuses are higher for ACOs that also demonstrate improved quality, but ACOs that do not meet quality metrics do not receive any bonus, even if they generated savings for Medicare. Bonuses and losses are shared equally by all members of the group.[8][9]
ACOs can be formed voluntarily by physicians, hospitals or—in the private market—insurers. Although the ACO provision of the Affordable Care Act pertains specifically to Medicare, some providers are forming ACOs for patients with private insurance as well, and 16 state Medicaid programs contracted with ACOs as of 2015. In fact, according to the journal Health Affairs, as of September 2015, the majority of the 23.5 million individuals served by ACOs were enrolled in private insurance or Medicaid. Medicare patients accounted for 7.8 million of the individuals in ACOs.[10]
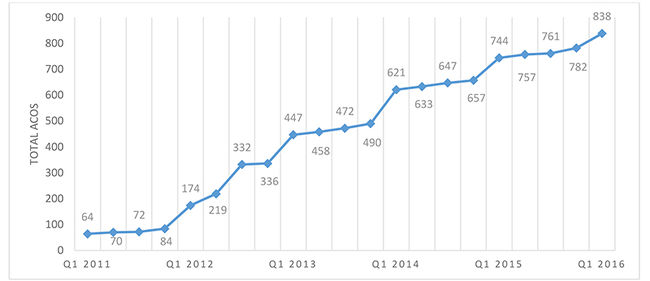
According to the Leavitt Partners, a healthcare research group, the number of ACOs in the United States has risen steadily since 2010. As of January 2015, there were 744 ACOs operating nationwide, with about 120 organizations becoming ACOs in 2014 alone. The chart below displays the growth of ACOs from 2011 to 2015.
Support
Supporters of pay-for-performance reimbursement say that under the dominant fee-for-service model, which reimburses physicians for every service provided, physicians may earn less by providing more cost-effective care. Thus, fee-for-service may provide a negative incentive for physicians to order more tests and complex services in order to receive a higher paycheck.[3]
| “ | Higher intensity of care does not necessarily result in higher-quality care, and can even be harmful."[11] | ” |
| —Health Affairs[2] | ||
Advocates say that by explicitly rewarding physicians for the quality of services rather than the volume of services, they will provide more efficient and effective care. The use of preventive services will increase and patients will have better "access to appropriate and timely care." Better care will result in better healthcare outcomes overall, they argue.[3][12]
At the same time, pay-for-performance arrangements will reduce the cost of care and mitigate rising healthcare spending, supporters say. Pay-for-performance solves the problems of both the underuse and overuse of healthcare by encouraging physicians to provide "the right care to the right patient at the right time." As patients receive more appropriate care and their health outcomes improve, they will require less complex care in the future, which will keep their healthcare costs down. Additionally, pay-for-performance will encourage physicians to use "less-expensive but equally effective treatments," also cutting down on health costs, advocates argue.[3][13]
Criticism
Overall, critics of pay-for-performance initiatives argue that there's little to no evidence that such programs are effective at improving patient outcomes. Some critics say that the programs are ineffective because they do not make any real structural changes and actually inject perverse incentives into the system. Pay-for-performance may cause physicians to narrow their focus on improving select measures on which they are scored, rather than improving overall care. Investing resources in these areas, which in some cases may require significant investments, may take away from other areas of need and incentivize "care that is not appropriate for certain patients."[14][15]
Other critics assert that pay-for-performance programs are ineffective because extrinsic financial rewards have little effect on individuals with intrinsic motivations, such as doctors who are "driven by the desire to reduce suffering." They point to prior pay-for-performance initiatives in education, another profession with similar intrinsic motivations, as a comparable demonstration of pay-for-performance failure. Some opponents argue that pay-for-performance programs "can actually backfire by demoralizing physicians and crowding out the intrinsic motivation they have to do good work."[15][16]
Opponents also argue that pay-for-performance programs harm hospitals that serve high numbers of low-income individuals, uninsured individuals, and minorities. They say that performance on quality achievement metrics can be "influenced by patient demographics and case complexity," and that hospitals that see a disproportionately higher number of low-income patients with complex health needs will perform more poorly on these metrics compared to other hospitals. Under pay-for-performance, such hospitals may be penalized. Such penalties would decrease the already-tight resources available to treat these patients and their quality of care would suffer as a result, exacerbating existing disparities.[2][14][15]
Recent news
The link below is to the most recent stories in a Google news search for the terms Pay for performance healthcare. These results are automatically generated from Google. Ballotpedia does not curate or endorse these articles.
See also
External links
- Health Affairs, "Health Policy Briefs: Pay-for-Performance"
- National Conference of State Legislatures, "Performance-Based Health Care Provider Payments- Health Cost Containment"
- Medicare.gov, "Linking quality to payment"
- The Heritage Foundation, "What Obamacare’s Pay-For-Performance Programs Mean for Health Care Quality"
Footnotes
- ↑ RAND Corporation, "Efforts to Reform Physician Payment: Tying Payment to Performance," February 14, 2013
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Health Affairs, "Health Policy Briefs: Pay-for-Performance," October 11, 2012
- ↑ 3.0 3.1 3.2 3.3 National Conference of State Legislatures, "Performance-Based Health Care Provider Payments," accessed April 18, 2016
- ↑ American Academy of Family Physicians, "Getting Rewards for Your Results: Pay-for-Performance Programs," March 11, 2004
- ↑ 5.0 5.1 5.2 5.3 Medicare.gov, "Linking quality to payment," accessed April 19, 2016
- ↑ Centers for Medicare and Medicaid Services, "Readmissions Reduction Program (HRRP)," accessed APril 19, 2016
- ↑ Medicare.gov, "Hospital-Acquired Condition Reduction Program," accessed April 19, 2016
- ↑ Politico, "Understanding Obamacare: POLITICO's Guide to the Affordable Care Act," accessed October 21, 2015
- ↑ Health Affairs, "Health Policy Brief: Next Steps for ACOs," January 13, 2012
- ↑ Health Affairs Blog, "ACO Results: What We Know So Far," May 30, 2014
- ↑ Note: This text is quoted verbatim from the original source. Any inconsistencies are attributable to the original source.
- ↑ American Academy of Family Physicians, "Pay-For-Performance," accessed April 19, 2016
- ↑ U.S. Department of Health and Human Services, "What is Health Care Quality and Who Decides?" March 18, 2009
- ↑ 14.0 14.1 The Heritage Foundation, "What Obamacare’s Pay-For-Performance Programs Mean for Health Care Quality," November 20, 2013
- ↑ 15.0 15.1 15.2 Harvard Business Review, "Doubts About Pay-for-Performance in Health Care," October 9, 201
- ↑ Physicians for a National Health Program, "Medicare’s pay-for-performance incentives unfairly penalizing safety-net hospitals: Annals of Internal Medicine editorial," September 7, 2015